6 Ways to Manage Insulin Resistance Symptoms
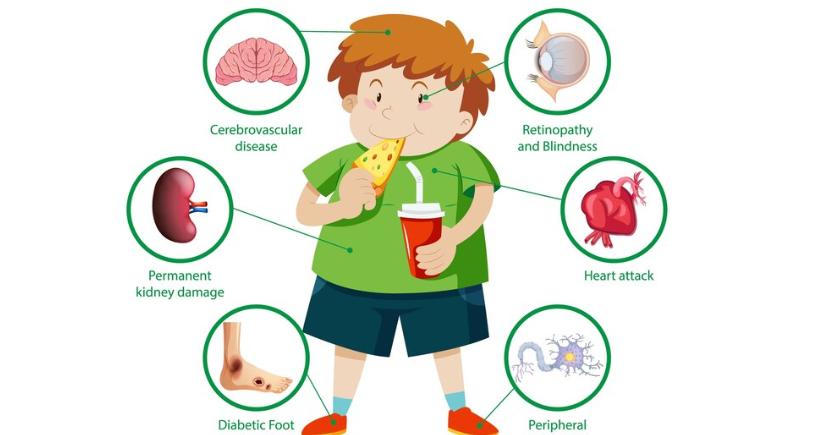
Type 2 diabetes, a major diet-induced insulin resistance that is the scourge of modern society, affects young and old. It happens when the body cells fail to respond positively to the drug insulin that is expected to control blood sugar levels. This can extend to high blood sugar and raise the danger of type 2 diabetes, cardiovascular diseases and other metabolic illnesses. Insulin resistance is a chronic disease. Its symptoms should be diagnosed and treated to avoid further health complications.
Understanding insulin resistance and its symptoms
Most cases of insulin resistance do not demonstrate symptoms that make it easy to diagnose at an early stage. Some common insulin resistance symptoms include:
- Lethargy or tiredness that does not seem to be relieved by rest or adequate sleep
- Abdominal obesity or weight gain that has not been caused by a specific medical condition
- Greed for foods and sweets and a general feeling of hunger
- Thickened skin patches, often under the armpits or on the neck (acanthosis nigricans)
- Usually lean and finding it hard to shed a pound despite their efforts to do so
- Females with insulin resistance symptoms mainly suffer from polycystic ovary syndrome (PCOS)
- Some of the symptoms that women who have
- PCOS face include irregular periods, hirsutism and acne. These are all the results of insulin resistance
Causes for insulin resistance
- Lifestyle factors: Poor diet, coupled with physical inactivity, leads to obesity. A poor diet comprises high-density, processed foods, sugars and unhealthy fats and oils.
- Obesity: Fat, specifically the abdominal visceral fat, impairs the normal functioning of insulin.
- Genetics: However, the presence of comorbidity with type 2 diabetes or other metabolic diseases, a history of which in the family, may lead to an increase in the risk.
- Hormonal imbalances: There are certain phenomena, such as PCOS and hormonal fluctuations during pregnancy. For example, it can negatively affect insulin resistance.
- Chronic stress and poor sleep: These factors may raise cortisol levels and, with time, affect insulin function in the body.
Effective ways to manage insulin resistance symptoms
Although insulin resistance may seem daunting, several strategies can help manage its symptoms and improve overall health:
- Adopt a balanced diet: A healthy diet is the foundation of treating Insulin Resistance. Eat foods directly from the farm or in their natural form to prevent the fluctuation of blood sugar. Key dietary tips include:
- Consume raw vegetables and fruits, beans, peas, and wholegrain foods.
- Choose healthier items like chicken, fish, tofu and beans.
- Eat nuts, seeds, avocados and olive oil.
- Steer clear of foods such as sweets, candy and snacks that contain high levels of simple sugars, refined carbohydrates and trans fatty acids.
- Regular physical activity: Exercise helps to upgrade insulin sensitivity because muscles are able to take up glucose. Ideally, a total of three types of activity, such as aerobic exercises, are walking, cycling, swimming and strength training activities. Just a simple exercise regime, like 30 minutes’ walk, can reduce or help fight the disease.
- Maintain a healthy weight: Losing even small amounts of weight, about 5–10 per cent of your starting weight, can lead to a better control of insulin resistance symptoms.
- Prioritising sleep: Lack of sleep and stress, in particular, lead to higher levels of insulin resistance. One should go to bed at the same time each day and avoid caffeine or any form of stress-relieving measures such as Yoga, meditation or deep breathing.
- Medications: Sometimes, however, this type of change may not be sufficient. Medications for insulin resistance include metformin and other drugs to reduce blood sugar and enhance the receptiveness of the body’s cells to insulin. Patients should seek the advice of a healthcare professional to receive specific advice about diagnosis, treatment and medication.
- Managing underlying conditions: Insulin resistance is commonly accompanied by other diseases, including PCOS, hypertension and high cholesterol. Specific treatment for these problems may also increase insulin sensitivity even further, in addition to making necessary lifestyle changes.
Conclusion
This is a tough situation, but one that is not in itself impossible to deal with, given the right interventions to take. If insulin resistance signs are detected in early stages, especially in females with PCOS, the health of the patient can be improved if the sources of insulin resistance are treated. Control of carbohydrate intake, a proper diet and proper exercise, reduced stress, and timely medical treatments can positively improve the sensitivity to insulin and thus protect from long-term effects. With this kind of lifestyle adjustment and getting professional advice, it is possible for one to fight insulin resistance and not allow it to take a toll on their health. Little changes at the present can result in a better and stronger coming year.