Deciphering Asherman’s Syndrome: Symptoms and Treatment
The implication of Asherman’s syndrome can be significantly complex since it triggers many complications that may affect every aspect of a woman’s life. This blog Breaks down explaining the symptoms, causes and treating of Asherman’s syndrome.
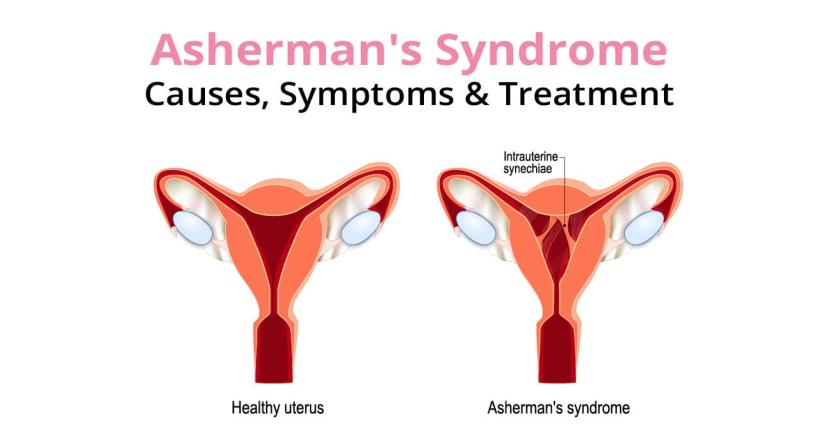
Recently the disease called Asherman’s syndrome which is also referred to as intrauterine adhesions or intrauterine synechiae, is growing, which is characterized by the presence of a scar in the uterus or cervix cavity. This syndrome is well experienced after uterine surgery and curettage. The syndrome triggers, whenever a patient is infected with tuberculosis or schistosomiasis leading to the formation of adhesion within the uterine cavity.
Causes
Primarily, Asherman syndrome happens after a curettage procedure, which is performed to terminate the pregnancy or remove any unwanted tissue from the retained placenta post-delivery or to complete the incomplete miscarriage.
Post-gynaecological procedures can lead to surgical infections leading to adhesions.
The syndrome can also occur from pelvic inflammatory diseases and tuberculosis.
The scar tissue can also extend from the uterine cavity, causing adhesions.
Radiation treatment for cancer can damage the uterine lining and lead to the formation of scar tissue.
A procedure to treat heavy menstrual bleeding by destroying the uterine lining can result in Asherman syndrome.
Surgeries to remove fibroids, polyps, or treat congenital uterine anomalies can sometimes result in scar tissue formation.
Manifestation or Symptoms
The symptoms of Asherman syndrome manifest after operation some of them include miscarriage, infertility, absence of menstruation, secondary amenorrhea.
A mild intrauterine adhesion may cause decreased menstruation, secondary amenorrhea, repeated abortion, uterine filling defect, abnormal obstetric history, abnormal hysterosalpingography image, gestational sac position abnormality and uterine volume reduction.
A moderate intrauterine adhesion may cause mild pelvic pain and persistent infection during pregnancy, miscarriage in early pregnancy, abnormal location of the placenta, and mild pain in the abdomen during or after giving birth.
Severe intrauterine adhesion may cause ectopic pregnancy, serous cell carcinoma of the uterus, and shock or even death of pregnant women.
Living with Asherman's Syndrome:
Living with Asherman's syndrome can be challenging, but effective treatment and proactive management can help. Always have an open communication with your gynaecologist. Speal about your concerns and treatment options. Seek emotional support from therapists or counsellors to navigate the emotional rollercoaster of this condition.
Diagnosis
The diagnosis involves hysteroscopy where a thin fibre-optic tube is passed through the cervix to allow for observation of the internal wall of the uterus. Blood test and other imaging procedures such as saline sonography or hysterosalpingography or two-dimensional sonography or MRI may be carried out to confirm the diagnosis.
Treatment and management
Surgical Intervention: Surgical treatment will be focussed on removing the scar tissue under the operation of a surgeon who has prior knowledge and experience in hysteroscopy or hysteroscopic adhesiolysis possibly with the help of sonographic or laparoscopic assistance.
Preoperative and Postoperative Care: Estrogenic preparation may be given orally or delivered transdermal or intramuscularly before and after surgery to minimize scar tissue and the subsequent utilization of estrogen to stimulate endometrial regeneration.
Use of Devices: In some case the use of intraoperative devices is selected to prevent the sticking of uterine walls and help to reduce formation of scar tissue. In such cases special attention is given to these devices to avoid the deleterious effects of pressure on the uterine wall muscle.
Prescription of Antibiotics: If an infection is suspected, antibiotics can help prevent further scarring
Experimental Treatments: They include protocols that involve stem cell transplants extracted from the patients’ blood cells or amniotic tissue and cell lines, which demonstrated the ability to regenerate endometrium. More research has to be carried out to determine the effectiveness, side effects and outcomes of such procedures.
Adhesive Gels: Synthetic hyaluronidase containing adhesive gels are useful in remediating adhesion recurrence though the full benefits have not been established.
Follow-up: Follow-up evaluation should be done one to two weeks after surgery to remove any recurrent adhesions.
Prevention and Management:
While there's no guaranteed way to prevent Asherman's syndrome, several steps can minimize the risk:
- Minimally invasive procedures: Opting for minimally invasive surgeries, when possible, reduces the risk of scarring.
- Careful post-procedural care: Following post-operative instructions diligently minimizes the chance of infection.
- Early diagnosis and treatment: Prompt medical attention can help prevent the condition from progressing.
Even though Asherman's syndrome can be frightening, it is not fatal. Many women regain their menstrual health and even become pregnant with the right diagnosis and therapy. Never forget that you are not traveling alone. Seek advice from licensed healthcare providers and maintain your optimism that there is a way to recover and have a happy life.
Popular Searches :
Hospitals: Cancer Hospital in Delhi | Best Heart Hospital in Delhi | Hospital in Amritsar | Hospital in Ludhiana | Hospitals in Mohali | Hospital in Faridabad | Hospitals in Gurgaon | Best Hospital in Jaipur | Hospitals in Greater Noida | Hospitals in Noida | Best Kidney Hospital in Kolkata | Best Hospital in Kolkata | Hospitals in Rajajinagar Bangalore | Hospitals in Richmond Road Bangalore | Hospitals in Nagarbhavi Bangalore | Hospital in Kalyan West | Hospitals in Mulund | Best Hospital in India | | Cardiology Hospital in India | Best Cancer Hospital in India | Best Cardiology Hospital in India | Best Oncology Hospital In India | Best Cancer Hospital in Delhi | Best Liver Transplant Hospital in India
Doctors: Dr. Rana Patir | Dr. Rajesh Benny | Dr. Rahul Bhargava | Dr. Jayant Arora | Dr. Anoop Misra | Dr. Manu Tiwari | Dr. Praveer Agarwal | Dr. Arup Ratan Dutta | Dr. Meenakshi Ahuja | Dr. Anoop Jhurani | Dr. Shivaji Basu | Dr. Subhash Jangid | Dr. Atul Mathur | Dr. Gurinder Bedi | Dr. Monika Wadhawan | Dr. Debasis Datta | Dr. Shrinivas Narayan | Dr. Praveen Gupta | Dr. Nitin Jha | Dr. Raghu Nagaraj | Dr. Ashok Seth | Dr. Sandeep Vaishya | Dr. Atul Mishra | Dr. Z S Meharwal | Dr. Ajay Bhalla | Dr. Atul Kumar Mittal | Dr. Arvind Kumar Khurana | Dr. Narayan Hulse | Dr. Samir Parikh | Dr. Amit Javed | Dr. Narayan Banerjee | Dr. Bimlesh Dhar Pandey | Dr. Arghya Chattopadhyay | Dr. G.R. Vijay Kumar | Dr Ashok Gupta | Dr. Gourdas Choudhuri | Dr. Sushrut Singh | Dr. N.C. Krishnamani | Dr. Atampreet Singh | Dr. Vivek Jawali | Dr. Sanjeev Gulati | Dr. Amite Pankaj Aggarwal | Dr. Ajay Kaul | Dr. Sunita Varma | Dr. Manoj Kumar Goel | Dr. R Muralidharan | Dr. Sushmita Roychowdhury | Dr. T.S. MAHANT | Dr. UDIPTA RAY | Dr. Aparna Jaswal | Dr. Ravul Jindal | Dr. Savyasachi Saxena | Dr. Ajay Kumar Kriplani | Dr. Nitesh Rohatgi | Dr. Anupam Jindal |
Specialties: Heart Lung Transplant | Orthopedic | Cardiology Interventional | Obstetrics & Gynaecology | Onco Radiation | Neurosurgery | Interventional Cardiology | Gastroenterologist in Jaipur | Neuro Physician | Gynecologist in Kolkata | Best Neurologist in India | Liver Transfer



















