Peripheral Artery Disease: Understanding the Condition
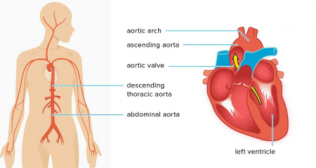
Peripheral artery disease (PAD) refers to plaque buildup in a person’s leg arteries. A person’s leg arteries transport oxygen and nutrient-rich blood from a person’s heart to their arms and legs. Alternative names for this are peripheral vascular disease/peripheral arterial disease.
When a person suffers from peripheral artery disease, plaque (made of fat, cholesterol, as well as other substances) gradually forms inside the person’s artery walls. Slowly, this plaque narrows the person’s arteries. This plaque is also called atherosclerosis.
Blood clots can form surrounding the plaque, making a person’s artery even narrower.
If plaque or a blood clot narrows/clogs person's arteries, blood can’t get through to nourish organs as well as other tissues. This causes harm ― and eventually death (gangrene) ― to the tissues below the blockage. This happens most often with a person’s toes as well as feet.
In this blog, let us delve into the symptoms, causes and risk factors, as well as treatment and ways of managing PAD:
What are the usual symptoms of peripheral artery disease?
Symptoms of peripheral artery disease comprise:
- A burning or aching pain in person's feet as well as toes while resting, especially at night while lying flat.
- Cool skin on person's feet.
- Redness/other color alteration of person's skin.
- More frequent skin along with soft tissue infections (usually in person's feet/ legs).
- Toe as well as foot sores that don’t heal.
Half of the individuals suffering from peripheral vascular disease don’t display any symptoms. PAD can build up over a lifetime. Symptoms may not become obvious until later in life. For many individuals, symptoms won’t appear until their artery narrows by 60% or more.
What is the most predominant cause of peripheral artery disease?
Atherosclerosis that develops in the arteries of a person’s legs — or, less commonly, in their arms — causes peripheral arterial disease. Like atherosclerosis in a person’s heart (coronary) arteries, a collection of fatty plaque in person's blood vessel walls causes peripheral vascular disease. As plaque builds up, a person’s blood vessels get narrower and narrower, until they’re blocked.
Risk factors for peripheral artery disease
- Utilization of tobacco products (the most potent risk factor).
- Suffering from diabetes.
- Being 50 and older.
- Having a personal/family history of heart/blood vessel disease.
- Having elevated blood pressure (hypertension).
- Having elevated cholesterol (hyperlipidemia).
- Having abdominal obesity.
- Having a blood clotting disorder.
- Suffering from renal disease (both a risk factor as well because of PAD).
Treatment of peripheral artery disease
Lifestyle changes, medicines and procedures can treat PAD.
The two primary goals of peripheral artery disease treatments are:
- Alleviating chances of cardiovascular events.
- Improving a person’s quality of life by easing the pain that happens with walking.
Lifestyle alterations
Treatment of PAD begins with making lifestyle changes to reduce person's risk factors. Alterations one can make to manage their condition comprise:
Quit usage of tobacco products and enquire about tobacco cessation programs.
A person can consume a balanced diet that’s high in fiber as well as low in cholesterol, fat and sodium. Limit fat to 30% of their total daily calories. Saturated fat should be responsible for no more than 7% of their total calories. Refrain from trans fats, comprising products made with partially hydrogenated as well as hydrogenated vegetable oils.
Exercise
Begin a regular exercise program, like walking. Walking can help treat PAD. Individuals who walk regularly can improve the distance they’re able to walk prior to their legs hurt.
Manage other health conditions, like elevated blood pressure, diabetes/ elevated cholesterol.
Individuals can keep their stress level low. Exercise, yoga as well as meditation may help with this.
Practice good foot and skin care to avoid infection and reduce the risk of complications.
Medicines
They can help people with conditions like elevated blood pressure (antihypertensive medications), elevated cholesterol (statin medications), as well as diabetes. These medications treat the risk factors of PAD and decrease a person’s risk of stroke and heart attack.
A person’s healthcare provider may prescribe an antiplatelet medication like aspirin/clopidogrel. They may also prescribe cilostazol to improve a person’s walking distance. This medication aids individuals with intermittent claudication exercise longer before they get leg pain.
Supervised exercise programs
A supervised exercise program will enhance the symptoms of pain in a person’s legs with walking, permitting them to walk farther. A structured program typically comprises walking on a treadmill in a supervised setting a minimum of three times per week.
Individuals suffering from PAD should also walk at home for a minimum of 30-60 minutes every day. The usual prescription is referred to as the “Start/Stop” exercise.
Minimally invasive/surgical treatments
For a few individuals with more severe PAD, leg pain may still cause problems in routine life, even post a few months of exercise as well as medications. In more severe cases, people must improve their blood flow to get rid of pain at rest or heal a wound.
More advanced PAD that’s causing critical pain and restricted mobility may require endovascular (minimally invasive) or surgical treatment. Few heart disease treatments also treat peripheral artery disease, comprising:
- Angioplasty
- Stents
- Peripheral artery bypass surgery
- Atherectomy
In a nutshell, Peripheral artery disease (PAD) poses significant risks to vascular health, particularly in the lower limbs, where plaque buildup can severely restrict blood flow. Lifestyle modifications like stopping smoking, adopting a healthy diet, as well as regular exercise play major roles in reducing cardiovascular risks associated with PAD. Medicines to control blood pressure, cholesterol levels, and blood clotting are essential components of treatment. In more severe cases, minimally invasive procedures or surgery may be necessary to restore sufficient blood flow and alleviate symptoms. Managing PAD requires a comprehensive approach to improve quality of life as well as alleviate the likelihood of cardiovascular events.
Popular Searches :
Hospitals: Cancer Hospital in Delhi | Best Heart Hospital in Delhi | Hospital in Amritsar | Hospital in Ludhiana | Hospitals in Mohali | Hospital in Faridabad | Hospitals in Gurgaon | Best Hospital in Jaipur | Hospitals in Greater Noida | Hospitals in Noida | Best Kidney Hospital in Kolkata | Best Hospital in Kolkata | Hospitals in Rajajinagar Bangalore | Hospitals in Richmond Road Bangalore | Hospitals in Nagarbhavi Bangalore | Hospital in Kalyan West | Hospitals in Mulund | Best Hospital in India | | Cardiology Hospital in India | Best Cancer Hospital in India | Best Cardiology Hospital in India | Best Oncology Hospital In India | Best Cancer Hospital in Delhi | Best Liver Transplant Hospital in India
Doctors: Dr. Rana Patir | Dr. Rajesh Benny | Dr. Rahul Bhargava | Dr. Jayant Arora | Dr. Anoop Misra | Dr. Manu Tiwari | Dr. Praveer Agarwal | Dr. Arup Ratan Dutta | Dr. Meenakshi Ahuja | Dr. Anoop Jhurani | Dr. Shivaji Basu | Dr. Subhash Jangid | Dr. Atul Mathur | Dr. Gurinder Bedi | Dr. Monika Wadhawan | Dr. Debasis Datta | Dr. Shrinivas Narayan | Dr. Praveen Gupta | Dr. Nitin Jha | Dr. Raghu Nagaraj | Dr. Ashok Seth | Dr. Sandeep Vaishya | Dr. Atul Mishra | Dr. Z S Meharwal | Dr. Ajay Bhalla | Dr. Atul Kumar Mittal | Dr. Arvind Kumar Khurana | Dr. Narayan Hulse | Dr. Samir Parikh | Dr. Amit Javed | Dr. Narayan Banerjee | Dr. Bimlesh Dhar Pandey | Dr. Arghya Chattopadhyay | Dr. G.R. Vijay Kumar | Dr Ashok Gupta | Dr. Gourdas Choudhuri | Dr. Sushrut Singh | Dr. N.C. Krishnamani | Dr. Atampreet Singh | Dr. Vivek Jawali | Dr. Sanjeev Gulati | Dr. Amite Pankaj Aggarwal | Dr. Ajay Kaul | Dr. Sunita Varma | Dr. Manoj Kumar Goel | Dr. R Muralidharan | Dr. Sushmita Roychowdhury | Dr. T.S. MAHANT | Dr. UDIPTA RAY | Dr. Aparna Jaswal | Dr. Ravul Jindal | Dr. Savyasachi Saxena | Dr. Ajay Kumar Kriplani | Dr. Nitesh Rohatgi | Dr. Anupam Jindal |
Specialties: Heart Lung Transplant | Orthopedic | Cardiology Interventional | Obstetrics & Gynaecology | Onco Radiation | Neurosurgery | Interventional Cardiology | Gastroenterologist in Jaipur | Neuro Physician | Gynecologist in Kolkata | Best Neurologist in India | Liver Transfer