Understanding Melena: What Does It Mean When You Have Dark Stools?
Understanding melena
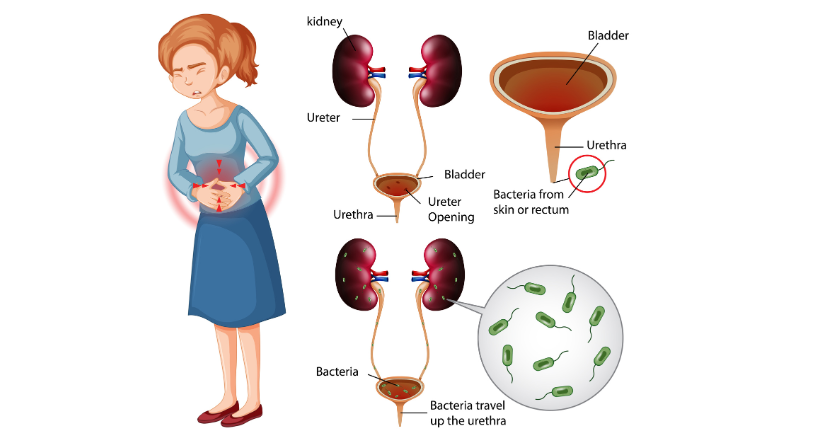
Melena often resembles haematochezia. However, the site and rate of bleeding differ in both cases. Haematochezia is characterised by bleeding from the lower gastrointestinal tract, such as the sigmoid colon or rectum, which is commonly associated with the passage of bright red blood. Typically, enzymes in the digestive system would break down the blood, changing its colour. In haematochezia, the bleeding happens quickly, and blood moves through the intestine too fast. However, when the bleeding is fast, there isn’t enough time for this process to happen. As a result, the blood appears bright red when passed in the stool. This condition is called haematochezia. The bright red colour indicates that the blood is fresh and hasn’t been digested or broken down.
Melena happens when blood originates from more proximal sections of the GI tract, such as the small intestine, or when bleeding from a lower source happens slowly enough to allow for the enzymatic breakdown of haemoglobin. The resulting stool is often dark and tarry. This appearance of characteristic dark colour and tarry consistency indicates blood has sufficient time to undergo digestion and degradation in the intestinal lumen, which causes typical dark colour and tarry consistency. If blood transits through the intestines faster than 14 hours, the individual is more likely to present with haematochezia rather than melena.
Melena is frequently used to describe bleeding that occurs around the Treitz ligament, which physically represents the confluence of the duodenum and jejunum. However, this origin-based indicator is not completely trustworthy, as there are cases where melena can develop from gastrointestinal bleeding sources, depending on characteristics such as bleeding rate and intestinal transit time.
Is melena a medical emergency?
Melena is a sign of significant internal bleeding. Immediate care is required to rule out serious causes and prevent complications in future.
The patient should immediately seek medical attention after experiencing such an incident. The doctor may ask a series of questions to completely understand symptoms and medical history in case of suspected melena. Here are some of the common questions to be prepared when consulting a doctor when experiencing such an event.
- What colour is your stool?
- Does it look like tar particularly black and sticky?
- Are you having any alterations in the colour and texture of your stool?
- Do you have any complaints related to the abdomen?
- Have you had any episodes of vomiting, especially vomiting in blood or material that resembled coffee grounds, in the last week?
- Do you experience or have sensations of feeling lightheaded or dizzy?
- Do you have any past medical conditions in the gastrointestinal tract, for example, peptic ulcer, gastritis or reflux esophagitis?
- Are you a diabetic, or have you complained of any other illnesses, such as skin diseases or allergies?
- Are you on any medications, like non-steroidal anti-inflammatory drugs, iron supplements or bismuth subsalicylate?
- Could the colour of your stools be attributed to the foods you’ve eaten, such as black liquorice, blueberries or blood sausage?
- Do you have any known bleeding disorders?
- When the individual has promptly provided information to the above questions, it allows the doctor to determine the melena cause and guide further diagnosis and treatment.
Investigations
Individuals suspected of melena are advised to undergo several tests to determine the cause and provide treatment accordingly. Some of the parameters assessed include:
- Blood tests to measure complete blood count, urea and creatinine levels, liver function, and erythrocyte sedimentation rate
- Stool tests to determine the presence of blood to confirm melena
- Endoscopy testing to identify the source of bleeding, such as ulcers or varices
Further investigations
Individuals with new-onset melena may also undergo gastroscopy (OGD) for additional evaluation. This will not only potentially identify the source of melena but also enable definite therapies in specific circumstances (e.g., banding of varices).
Conclusion
Melena is suspected when the stool remains in the colon long enough for bacteria to break down the blood, turning it dark and tarry. Bleeding from the junction of the duodenum and jejunum is frequently associated with melena, though this is not necessarily a reliable sign. If dark, tarry stools are noticed, seek medical assistance immediately. Early examination is critical for identifying the underlying problem and immediately initiating suitable treatment.