Understanding Ventricular Tachycardia
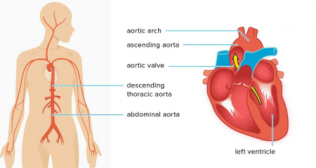
Ventricular tachycardia (VT) is a potentially life-threatening heart rhythm disorder characterized by abnormally fast heartbeats originating in the ventricles, the lower chambers of the heart. In a healthy heart, the electrical signals that control the heartbeat originate in the sinoatrial (SA) node, located in the right atrium, and travel through the atria and then the atrioventricular (AV) node before reaching the ventricles. VT occurs when the electrical signals initiate in the ventricles, causing them to contract very rapidly and inefficiently.
Symptoms of ventricular tachycardia may vary depending on the duration, rate, and underlying heart disease, and they can include:
- Palpitations: A sensation of rapid, strong, or irregular heartbeat.
- Chest pain or discomfort: Often described as pressure, squeezing, or burning.
- Shortness of breath: Due to the reduced ability of the heart to pump blood effectively.
- Dizziness or lightheadedness: Caused by inadequate blood flow to the brain.
- Loss of consciousness (syncope): In severe cases, VT can lead to fainting or collapse.
- Ventricular tachycardia can be categorized into sustained and non-sustained forms. Sustained VT lasts for more than 30 seconds or requires intervention to terminate, whereas non-sustained VT lasts for less than 30 seconds and often does not cause significant symptoms.
Treatment for ventricular tachycardia aims to:
- Stabilize the Patient: If the patient is experiencing hemodynamic instability (e.g., low blood pressure, loss of consciousness), immediate medical attention is required. In such cases, cardioversion (electric shock) may be used to restore a normal heart rhythm.
- Identify and Address Underlying Causes: VT often occurs in the presence of other heart conditions, such as coronary artery disease, cardiomyopathy, or heart failure. Treating these underlying causes is essential.
- Medications: Antiarrhythmic medications like amiodarone, lidocaine, or procainamide may be prescribed to control VT and reduce the risk of recurrence.
- Implantable Cardioverter-Defibrillator (ICD): For individuals at high risk of recurrent VT or sudden cardiac death, an ICD may be implanted. This device continuously monitors the heart's rhythm and can deliver an electric shock (defibrillation) to restore a normal rhythm if VT or ventricular fibrillation (a more chaotic and life-threatening rhythm) occurs.
- Catheter Ablation: In many cases, a procedure called catheter ablation may be performed. This involves the use of catheters to destroy or isolate the abnormal electrical pathways causing VT.
- Lifestyle Changes: Managing risk factors such as high blood pressure, smoking, excessive alcohol consumption, and obesity can help reduce the risk of VT.
It's essential for individuals with ventricular tachycardia to work closely with a cardiologist or electrophysiologist (a specialist in heart rhythms) to develop an appropriate treatment plan tailored to their specific condition and needs. Early diagnosis and treatment are crucial in managing VT and preventing complications.
Categories
Clear allMeet the doctor

- Cardiac Sciences | Electrophysiology
-
35 Years
-
2000