What is Fetal Echocardiography: Purpose, Benefits and Limitations
Introduction
Congenital heart disease (CHD) is a prevalent abnormality in newborns. The global prevalence of CHD is 8 per 1000 live births. Innovations in the before-birth diagnosis of cardiac abnormalities have resulted in a crucial decline in neonatal deaths related to these abnormalities. Fetal echocardiography plays a key role in diagnosing CHD. Let us learn more about the method of performing fetal echocardiography, its advantages, and indications!
What is Fetal Echocardiography?
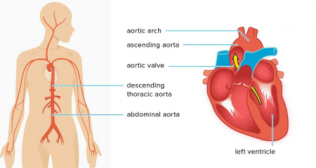
Fetal echocardiography (echo) is a non-invasive procedure that employs sound waves to evaluate the heart of a developing baby in terms of:
- Recognizing structural defects
- Checking for rhythm abnormalities
- Assessing the functional characteristics of the fetal heart
If a heart problem can be detected early, there is a higher chance that the treatment will work. This is because:
- In some instances, healthcare professionals may be able to treat the problem before birth.
- Healthcare professionals can prepare for problems during labor and delivery.
- An early delivery can be planned.
- Treatment may be performed as soon as the baby is born. This treatment might be medication or surgery.
Expressing Curiosity: Need for Fetal Echocardiography
Family History:
- A parent, sibling, or any other close family member had a cardiac defect or disease.
Health Conditions:
- Mother has diabetes (before pregnancy), Sjogren’s syndrome, lupus, or phenylketonuria.
- Mother is suffering from rubella during the first trimester of pregnancy.
Medications:
- Mother has taken medicines that can damage the baby’s developing heart, such as:
- Epilepsy drugs and prescription acne medications
- ACE inhibitors
- Mother has taken medicines that can damage the baby’s developing heart, such as:
Other Reasons:
- There are specific other reasons to suspect that the baby has a higher chance of heart problems.
- Mother has conceived using assisted reproductive technology.
- An amniocentesis depicted a chromosomal disorder.
Indications for Transforming a Routine Scan Into Fetal Echocardiography
- Asymmetry of the heart chamber
- Modified cardiac axis
- Arrhythmia
- Modified position of the fetal heart
- Abnormally enlarged fetal heart
Shedding Light on How the Test is Performed
Fetal echocardiography is performed while the baby is still in the womb. It is most often performed during the second trimester of pregnancy (at 18 to 24 weeks of pregnancy). The procedure is like that of a pregnancy ultrasound. The female will lie down for the procedure. The test can be performed on the belly (abdominal ultrasound) or through the vagina (transvaginal ultrasound).
In an abdominal ultrasound, the healthcare professional performing the test applies a clear, water-based gel on the belly. A hand-held probe is rubbed over the target area. The sound waves originating from the probe bounce off the fetal heart and create its image on a screen.
In a transvaginal ultrasound, a miniature probe is placed into the vagina. A transvaginal ultrasound can be performed in the early stages of pregnancy and generates a clearer image than an abdominal ultrasound.
Reaping the Benefits of Fetal Echocardiography
- Early Detection of Heart Defects: Heart defects can be diagnosed within as early as 18–20 weeks, enabling sufficient care for the baby in utero and at the time of delivery.
- Planning of Treatment: Early diagnosis permits healthcare professionals to plan suitable treatment. Collaboration with obstetric doctors ensures that treatment can be given in a timely manner and that the team is sufficiently prepared.
- Better Outcomes: Scientifically, early diagnosis and timely treatment critically enhance a child’s outcome without complications, decreasing the financial burden on the family due to a rapid recovery. Newborns often develop complications when CHD diagnosis is postponed. Heart conditions such as atrial septal defect, tetralogy of Fallot (an unusual condition caused by a combination of four heart defects present at the time of birth), ventricular septal defect, and aortic stenosis (aortic valve narrows and blood cannot flow normally), and more can now be entirely or satisfactorily treated.
What’s Next: After Fetal Echocardiography!
Healthcare professionals will look at the results of fetal echocardiography. Women might have to undergo more tests or procedures, including:
- Treatment: This may include medication or other procedures to treat fetal cardiac problems.
- Fetal Wellness Assessments: Women may be asked to calculate fetal movements to assess overall fetal health.
- Non-Stress Test: It examines fetal movement and heart rate.
- Biophysical profile (BPP): This tool is used to examine overall fetal health. It analyses heart rate, breathing, movement, tone of muscle, and the quantity of amniotic fluid.
- Ultrasound or Echocardiography: These tests are performed to confirm the diagnosis. They are also used to follow fetal growth, assess changes in fetal heart, and look for other problems.
- Amniocentesis: This test can detect chromosomal and genetic disorders and certain birth defects. The healthcare professional inserts a needle through the wall of the abdomen and uterus and into the amniotic sac. They then extract a sample of the amniotic fluid.
- Genetic Counseling: A counselor educates a woman about the risks of having a baby with genetic defects.
Limitations of Fetal Echocardiography
Certain heart defects cannot be seen before birth, even with fetal echocardiography. These comprise tiny holes in the heart or mild valve defects. Also, because it may not be possible to observe every part of the large blood vessels coming out of the baby’s heart, any potential problems in this aspect may go undetected. It may still be required to repeat the ultrasound of the baby’s heart after the delivery to validate the findings of fetal echocardiography and evaluate the previously inaccessible areas.
If the healthcare professional finds a problem in the fetal heart structure, a detailed ultrasound may be performed to check for other issues with the developing baby.
Fetal echocardiography plays a significant role in ensuring the well-being of fetuses with cardiac ailments, enabling the best possible care from birth.
Popular Searches :
Hospitals: Cancer Hospital in Delhi | Best Heart Hospital in Delhi | Hospital in Amritsar | Hospital in Ludhiana | Hospitals in Mohali | Hospital in Faridabad | Hospitals in Gurgaon | Best Hospital in Jaipur | Hospitals in Greater Noida | Hospitals in Noida | Best Kidney Hospital in Kolkata | Best Hospital in Kolkata | Hospitals in Rajajinagar Bangalore | Hospitals in Richmond Road Bangalore | Hospitals in Nagarbhavi Bangalore | Hospital in Kalyan West | Hospitals in Mulund |
Doctors: Dr. Rana Patir | Dr. Rajesh Benny | Dr. Rahul Bhargava | Dr. Jayant Arora | Dr. Anoop Misra | Dr. Manu Tiwari | Dr. Praveer Agarwal | Dr. Arup Ratan Dutta | Dr. Meenakshi Ahuja | Dr. Anoop Jhurani | Dr. Shivaji Basu | Dr. Subhash Jangid | Dr. Atul Mathur | Dr. Gurinder Bedi | Dr. Monika Wadhawan | Dr. Debasis Datta | Dr. Shrinivas Narayan | Dr. Praveen Gupta | Dr. Nitin Jha | Dr. Raghu Nagaraj | Dr. Ashok Seth | Dr. Sandeep Vaishya | Dr. Atul Mishra | Dr. Z S Meharwal | Dr. Ajay Bhalla | Dr. Atul Kumar Mittal | Dr. Arvind Kumar Khurana | Dr. Narayan Hulse | Dr. Samir Parikh | Dr. Amit Javed | Dr. Narayan Banerjee | Dr. Bimlesh Dhar Pandey | Dr. Arghya Chattopadhyay | Dr. G.R. Vijay Kumar | Dr Ashok Gupta | Dr. Gourdas Choudhuri | Dr. Sushrut Singh | Dr. N.C. Krishnamani | Dr. Atampreet Singh | Dr. Vivek Jawali | Dr. Sanjeev Gulati | Dr. Amite Pankaj Aggarwal | Dr. Ajay Kaul | Dr. Sunita Varma | Dr. Manoj Kumar Goel | Dr. R Muralidharan | Dr. Sushmita Roychowdhury | Dr. T.S. MAHANT | Dr. UDIPTA RAY | Dr. Aparna Jaswal | Dr. Ravul Jindal | Dr. Savyasachi Saxena | Dr. Ajay Kumar Kriplani | Dr. Nitesh Rohatgi | Dr. Anupam Jindal |
Specialities: Heart Lung Transplant | Orthopedic |