LVAD Heart Surgery
Overview
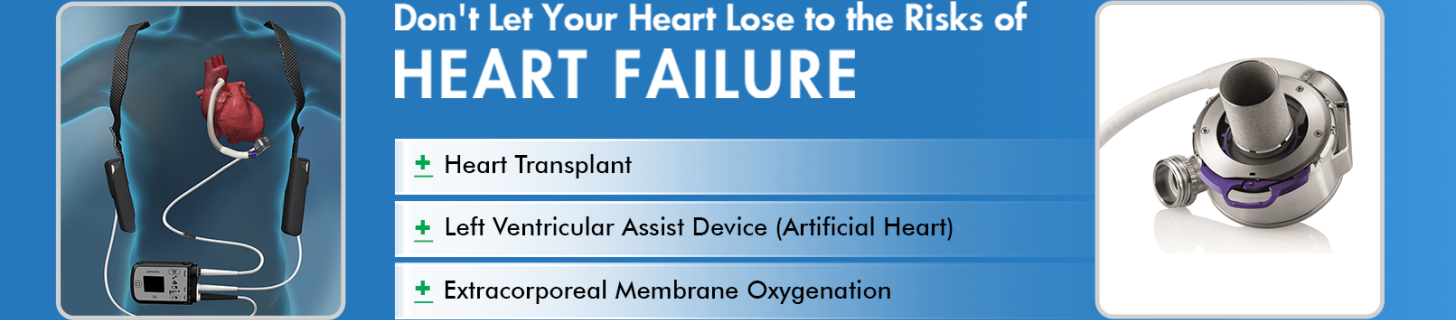
The left ventricular assist device (LVAD) refers to a supporting circulatory system. This is used to increase the survival rate and decrease the mortality in individuals with heart failure. It helps to pump the blood from the lower chambers of the heart to the remaining body parts. It is used either as temporary support before a heart transplant or as permanent support to pump blood.
LVAD is a durable mechanical circulatory support or continuous flow device. It is generally placed in the left ventricle and continuously supplies blood to other body parts. It is a lifesaving device in heart failure and is usually placed by doing an open-heart surgery.
Indications
LVAD is a mechanical pump that distributes blood to other body parts. Individuals considered for LVAD generally have severe heart failure symptoms, are on maximum medical support, or need respiratory or defibrillator support. It plays a vital role and is indicated in the following conditions:
- In individuals with heart failure and who are waiting for a donor, LVAD provides circulatory support till the donor is available and transplantation is done. This is called Bridge to transplant. LVAD pumps blood and supports the functioning of body parts.
- In individuals who are not eligible for heart transplants, LVAD is used as a permanent device to increase survival rates. This is called destination therapy, where the quality of life can be improved despite heart failure.
- For those with end-organ dysfunction due to heart failure, LVAD is used to stabilize the individual, improve renal function and nutritional status, and reduce hypertension.
- In case of temporary heart failure, LVAD supports the body by pumping blood till the heart returns to its function. This is called the Bridge to recovery.
Contraindications
It is not indicated in individuals with right heart failure. Right ventricular dysfunction can lead to insufficient left heart filling, causing further complications. When an individual has severe life-threatening conditions that affect the functioning of kidneys, lungs, and liver or has life-threatening neurological conditions that can increase the risk of morbidity and further complications.
LVAD is also not indicated when an individual has active bleeding complications due to decreased platelets. A condition called hypertrophy, which increases the size of the heart or has significant defects in the septae of the heart, is also not eligible for LVAD, which can cause difficulty in the placement of the device.
Before the Procedure
An individual needs surgery to get an LVAD. Before getting surgery, the healthcare professional assesses the severity of heart failure, considers other life-threatening conditions, estimates the functioning capacity of heart chambers, the safety of blood thinners to be taken, and assesses the support one has from the family. Based on these criteria, they consider the treatment with LVAD.
An individual's physical health will be assessed using blood tests, electrocardiograms, chest X-rays, and echocardiograms. These are done to determine the body functions and know the current health status. An Electrocardiogram is done to understand the electrical function of the heart, a chest X-ray is done to assess the size and shape of the heart, and an echocardiogram gives information about the structure of the heart, its valves, and blood flow through the heart.
A long, thin tube called the catheter is inserted in the neck and guided by X-rays to determine the pressure and blood flow in the heart. These tests are used to decide if LVAD is the right treatment choice.
During the Procedure
LVAD is done by open-heart surgery under anaesthesia. The entire procedure takes about four to six hours. Hair is removed from the surgical site, and the patient's body is prepared. Respiratory support is given through a ventilator. Heart function will be stopped temporarily and connected to a heart-lung bypass machine that carries out the function. A cut is made on the centre of the chest, and the chest bone is separated.
The main pump of LVAD is placed near the tip of the heart, and a cord is placed from a cut in the skin that connects the pump to the control unit and battery pack outside the body. As the LVAD starts functioning, an individual will be removed from the heart-lung bypass machine.
After the Procedure
An individual will be constantly monitored till the vitals stabilize and for any complications. Medications like antibiotics, painkillers, and blood thinners will be given to ward off infections and pain and prevent blood clots. Ventilator support for respiration will be taken for a few days. Instructions will be provided on LVAD care, such as cleaning the area, keeping the batteries charged, checking the controller for battery damage, and ensuring the proper functioning of the LVAD. Recovery time depends on the medical condition of the individual. Multiple follow-up appointments will be given to check the device's functioning and for any complications.
The Success of the Procedure
LVAD is considered successful if the quality of life of an individual is improved and the survival rate is increased. Healthy lifestyle changes like quitting smoking and alcohol, eating a nutritious diet, and exercising regularly increase the chances of success.
Risks and Complications
Some of the risks and complications linked with the procedure are the risk of bleeding after the surgery, the formation of blood clots, and infections. Risks associated with the device include malfunctioning when there is any damage to the wires, which needs immediate medical attention. Complications like right heart failure and kidney damage may develop as the left heart functioning increases after an LVAD.
Conclusion
Left ventricular assist devices (LVADs) are an advanced medical technology that increases the lifeline of individuals with severe heart failure. By providing circulatory support either as a bridge to transplantation or as destination therapy, LVADs significantly enhance survival rates as well as improve the quality of life for patients. LVAD improves cardiac function and increases survival, offering hope for those with advanced heart disease.